Study Population And Incidence Of Neoaf
A total of 791 patients were screened. Of these patients, 36 and 43 patients were excluded due to pre-existing AF and arrhythmia other than AF, respectively. The prevalence of pre-existing AF was 4.5% . The incidence of NeOAF was 35.1% . After excluding patients older than 90 years, with less than 3 days of ICU stay, missing or incomplete data, or having had major surgery within 2 weeks of sepsis, 503 eligible patients were evaluated based on the different AF status. Among these, 263 patients had no AF and 240 patients developed NeOAF after ICU admission. SR was restored in 165 patients and SR could not be restored in 75 patients as shown in Fig. 1.
What Was Aggressive Atrial Fibrillation Care In This Study
In order to keep the people in normal sinus rhythm in the EAST-AF Study, aggressive treatment meant that physicians could try any combination of the following three options:
1. An anti-arrhythmic medication like Dronedarone, Amiodarone, Flecainide, or Propafenone.
2. Cardioversion where the heart is shocked back into normal sinus rhythm.
3. Catheter ablation.
Reasons Why Sinus Rhythm Beats Atrial Fibrillation
Now that weve covered the basics of the study, lets get to what it showed. And below are the 4 reasons why normal sinus rhythm beats atrial fibrillation according to the EAST-AF Study.
1. Doing whatever it takes to keep your heart in normal sinus rhythm decreased your combined risk of something really bad happening by 21%. And really bad in this study was defined as a cardiac death, stroke/mini-stroke, or getting hospitalized for worsening heart failure or coronary artery disease.
2. Aggressive atrial fibrillation treatment resulted in many more hearts maintaining normal sinus rhythm. In fact, 85% of patients with aggressive treatment were in normal sinus rhythm a year later with only a slight decrease over time.
3. Having a goal of maintaining normal sinus rhythm decreased the risk of stroke by 35%.
4. Keeping your heart in rhythm was associated with a 28% less risk of a cardiac death.
Read Also: Simply Saline Allergy & Sinus Relief Nasal Mist
Heart Rate Between 60 Bpm And 100 Bpm
Sinus rhythm has a heart rate higher than 60 bpm and lower than 100 bpm. If heart rate is lower than 60 bmp it is called sinus bradycardia, if heart rate is higher than 100 bpm it is called sinus tachycardia.
Sinus rhythm:Minimum R-R interval and maximum R-R interval .
As sinus rhythm is regular if the distance between two QRS complex is larger than 3 big squares and less than 5 big squares, the heart rate is normal.
Special Situations Atrial Fibrillation
Atrioventricular Nodal Ablation and Permanent Pacing
When high doses of AV blocking drugs do not control the ventricular response rate in atrial fibrillation, AV nodal ablation offers another option. Atrial action potentials must traverse the AV node to reach the ventricle. AV node ablation destroys this connection. This results in complete heart block. The ventricular His-Purkinje system has an intrinsic rate of 30 to 40 beats per minute resulting in severe bradycardia after the AV node ablation, and a permanent pacemaker is required.
Vagally-mediated Atrial Fibrillation
Atrial fibrillation triggered by episodes of vagal stimulation has been well described . Disopyramide, an agent with significant anticholinergic activity, may be useful, although data are very limited.
Holiday Heart
Ingestion of large amounts of alcohol may trigger atrial fibrillation, even with a structurally normal heart. Clinicians refer to the familiar association of excessive alcohol intake and acute atrial fibrillation as holiday heart.
Atrial Fibrillation in Hypertrophic Obstructive Cardiomyopathy
Because disopyramide has significant negative inotropic effects, it may occasionally be useful for management of atrial fibrillation in patients with HOCM, although sotalol is more attractive.
Atrial fibrillation in Wolff-Parkinson-White
Procainamide is the appropriate therapy. Synchronized DC cardioversion is recommended for hemodynamic instability.
References:
You May Like: Polyp Cyst In Maxillary Sinus
How Does Atrial Fibrillation Affect My Body
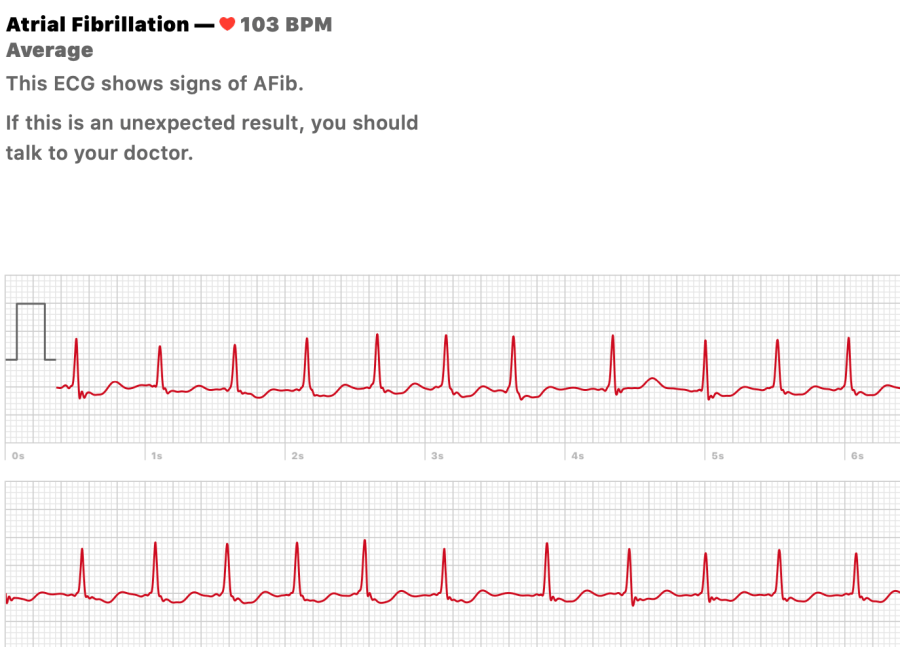
When youre in Afib, your hearts electrical system isnt working as it should. Your electrical impulses are chaotic, leading to an irregular and rapid heartbeat. When you feel your pulse isnt right, you might wonder whats going on inside your heart. Its helpful to learn more about the differences between a normal heartbeat and what happens when youre in Afib.
How your heart normally works
Your heart pumps blood to the rest of your body. During each heartbeat, your two atria contract, followed by your two lower chambers . These actions, when timed perfectly, allow your heart to work as an efficient pump. Your hearts electrical system controls the timing of your hearts contractions. And your sinoatrial node is normally in charge of that electrical system. This node is located in your right atrium. When your SA node fires an impulse, electrical activity spreads through your right and left atria . Both atria then contract and force blood into your ventricles.
The impulse then travels to the atrioventricular node, located near the middle of your heart. From there, the impulse moves to your ventricles, causing them to contract and pump blood out of your heart to your lungs and the rest of your body. This process repeats with every heartbeat. The SA node directs the timing of the electrical impulses and keeps your heart pumping smoothly.
What happens when youre in Afib
How Likely Is It That Treatment To Restore The Heart Rhythm Will Be Successful In The Long Term
Many people who have had successful cardioversion develop again. According to studies, this happens within a year in up to 80 out of 100 people. The success rate can be improved somewhat by taking anti-arrhythmic medication over the longer term. But it is only rarely possible to stop the heart rhythm becoming irregular again at some point.
Anti-arrhythmics can cause a number of side effects when taken over a longer period of time. For instance, in 5 out of 100 people they cause heart rhythm problems that may sometimes be life-threatening. Other possible side effects include vision problems, increased skin sensitivity to light, as well as nausea, vomiting and diarrhea. The side effects go away again if you stop taking the medication.
Read Also: Best Over The Counter Medicine For Sinus Congestion And Pressure
My Take On This Study
This study fits nicely with our experience in taking care of tens of thousands of patients with atrial fibrillation over the last 30 years. It also validates our previous studies showing that you have to hit atrial fibrillation early and hard if you want to maintain normal sinus rhythm long-term. Also, our research has shown that maintaining normal sinus rhythm may prevent an early death, strokes, and dementia which is right in line with the EAST-AF Study.
If you want to see my additional comments, I was interviewed in this news report on the EAST-AF Study:
https://www.healio.com/news/cardiology/20200829/eastafnet-4-early-rhythm-control-for-af-reduces-risk-for-poor-cv-outcomes
Did you like the photograph with this article? It shows my daughter perfectly in rhythm doing a handstand on the beach with two of my sons watching her from the water.
Choosing A Treatment Strategy
The decision regarding whether or not to have treatment to restore your heart rhythm is ultimately a personal decision. It will depend on how you feel about the pros and cons of the treatment. Many medical societies only recommend cardioversion if other treatments arent effective enough.
It is best to talk with your doctor about which treatment strategy is suitable for you. Regardless of whether you decide to have treatment to control your heart rate or treatment to restore your heart rhythm, the decision wont necessarily be final: Your situation may change over time, leading to a change in treatment strategy.
You May Like: Ways To Cure Sinus Congestion
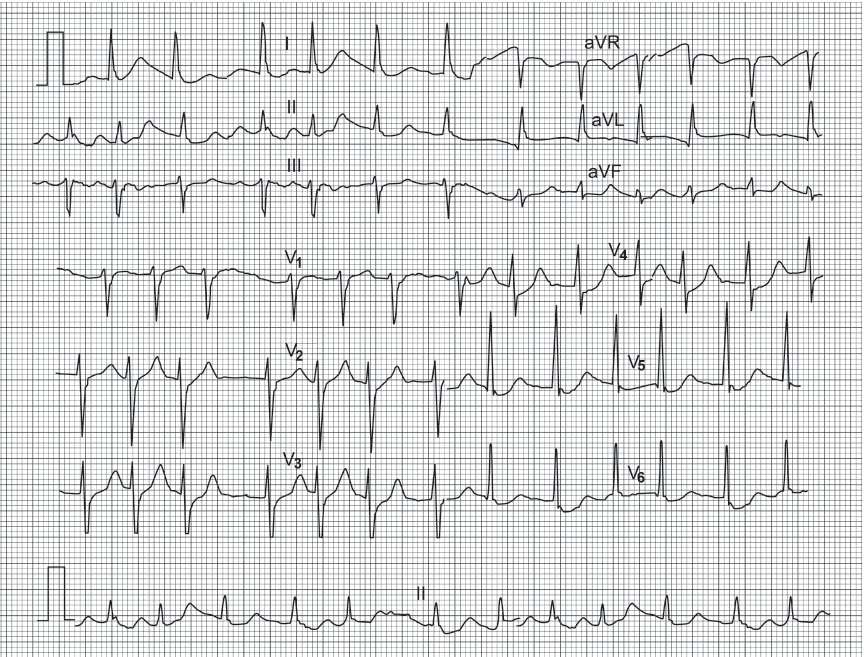
Study Design And Participants
This retrospective study is conducted with a database of ECGs collected from a large cohort of 122,394 patients at La Princesa University Hospital between May 5, 2010 and February 4, 2019. The Clinical Ethics Committee from Hospital La Princesa approved this study with a waiver of obtaining informed consent from patients. All methods were performed in accordance with the relevant guidelines and regulations. The initial database contains 296,022 12-lead ECGs from 122,394 patients. Each ECG is measured with a sample frequency of 500 Hz and lasts ten seconds. ECGs have been processed by the Philips 12-Lead Algorithm that provides an automatic interpretation of rhythm and extracts discrete variables related to global and lead-specific attributes of the signal. Variables and raw signals are stored in XML files together with information related to patients. Signals are preprocessed to maintain frequencies between 0.7 and 90 Hz and remove frequencies around 50 Hz, noisy due to power supply. We exclude from the study patients with no information about age and patients with only one recorded ECG, since they are not helpful in our analysis.
Diagnosis Of Sepsis And Its Severity
According to Surviving Sepsis Campaign recommendations, information on infection sites and sepsis-induced acute organ dysfunction, including neurologic, circulatory, respiratory, renal, hepatic, and hematologic dysfunction was collected. Scores of severity-of-disease classification systems including the Acute Physiology and Chronic Health Evaluation II and Sequential Organ Failure Assessment were recorded for each individual on ICU admission .
Don’t Miss: Sinus Infection Not Getting Better
Management Of Neoaf In Patients With Sepsis
We reviewed 240 eligible patients with NeOAF. Among these 240 patients, SR was restored in 165 patients , and SR could not be restored in 75 patients . Treatments received by patients with NeOAF are shown in Table 4. Beta-blockers and amiodarone were the most commonly used in patients with NeOAF and sepsis, followed by non-DHP CCBs and digitalis glycosides. Electrical cardioversion was performed in only eight patients. There were no significant differences in pharmacological therapies and electrical cardioversion between the NeOAF to SR and NeOAF to AF groups.
What Causes Atrial Fibrillation To Start
Changes or damage to your hearts tissue and electrical system cause atrial fibrillation. Usually, coronary artery disease or high blood pressure causes those changes. Often a trigger heartbeat causes atrial fibrillation to begin. But sometimes its hard to know the cause of that triggered heartbeat. For some people, there is no identifiable cause. Research is constantly providing new information to help us learn more about the
Afib often runs in families. So, if a close family member has Afib, you have a family history and therefore a higher chance of developing it, too.
Can atrial fibrillation be caused by anxiety?
We dont fully know the connections between atrial fibrillation and anxiety. Research has identified Afib as a cause of anxiety . But few studies have explored anxiety as a cause of Afib. We do know that anxiety can raise your risk of cardiovascular disease and causes a 48% higher risk of cardiac death. However, we need more research to find out if anxiety disorders can cause Afib.
Recommended Reading: How To Break Up Severe Sinus Congestion
Epidemiology And Clinical Consequences Of Af
The prevalence of AF continues to rise in Western nations. Recent research suggests that in the United States, for example, an estimated 2.3 million people have AF. The overall lifetime prevalence of the arrhythmia is approximately one in six individuals for the general population, and roughly one in four for people > 40-years-old.
AF is a major cause of morbidity and mortality, and is associated with a 1.51.9 relative risk of mortality and a relative risk of up to 4.5 for ischaemic stroke., Indeed, AF accounts for nearly 15% of all cerebral thrombo-embolic events. AF is also frequently complicated by heart failure, and the presence of both conditions may worsen the overall prognosis. The adverse haemodynamic effects of AF stem not only from the loss of atrial contraction and the rapidity and irregularity of ventricular contraction but also from the induction of tachycardia cardiomyopathy. Whether AF in the setting of heart failure is related to an increased risk of mortality is unknown at present.
Hypothesis Of Rhythm Control Strategy In Patients With Sepsis And Neoaf
The development of NeOAF could lead to deteriorated hemodynamic status during sepsis. The occurrence of NeOAF makes the disease more complicated and makes treatment during sepsis or septic shock more challenging because of adverse cardiovascular effects including rapid heart rate, irregular rhythm, loss of atrial systole, and neurohormonal activation. In the acute phase, both tachycardia and loss of atrial systole caused by AF could reduce the cardiac output, further destablizing patients with sepsis. Subsequently, the burden of NeOAF in patients with sepsis may result in acute heart failure . Moreover, atrial stasis and sepsis-related coagulopathy could lead to systemic embolization and an increased risk of ischemia stroke .
AF itself has been found to subsequently generate an inflammatory response that further enhances atrial remodeling and perpetuates arrhythmia. Previous studies have proposed that restoration and maintenance of SR in patients with AF could result in gradually decreasing CRP, indicating that AF initiates inflammation . Therefore, inflammation could promote AF and vice versa. To stop the vicious cycle between inflammation and AF, the early management of NeOAF by rhythm control may be beneficial in patients with sepsis.
Also Check: Advil Cold And Sinus For Allergies
How Common Is Atrial Fibrillation
Some researchers have called Afib the new cardiovascular disease epidemic of the 21st century. Afib is especially common among older adults. Over 33 million people age 55+ have been diagnosed globally. Estimates predict that 12 million people in the U.S. will have Afib by 2030. Afib causes nearly half a million yearly hospitalizations in the U.S. and leads to more and more deaths with each passing year.
Blood Thinners And Anticoagulation
Instead of an electrical cardioversion, your physician may opt to perform a chemical cardioversion. A chemical cardioversion is administered via antiarrhythmic medications typically through an intravenous route . The procedural preparation would be the same, with continuous electrical and respiratory monitoring after injection of the agent. These medications typically take longer to convert a patient to normal sinus rhythm, and if unsuccessful, your physician may opt to electrically cardiovert you the same day. Your physician will discuss the risks and benefits of both scenarios, including the small incidence of pro-arrhythmias with the use of intravenous antiarrhythmic medications.
Don’t Miss: Advil Cold And Sinus Directions For Use
Sinus Rhythm With 2nd Or 3rd Degree Av Blocks
Atria are depolarizated by sinus node, but some or all stimuli are not conducted to the ventricles.
In 2nd degree AV block not all sinus P waves are followed by QRS complexes because there is an intermittent failure of the AV conduction.
In complete AV block sinus P waves are dissociated from QRS complexes. No P waves are conducted to the ventricles because there is a complete block of the AV conduction.
It may be described as Sinus Rhythm with Second or Third degree AV Block.
What Is Atrial Fibrillation
Atrial fibrillation is an irregular heart rhythm that begins in the upper of your heart. If you have atrial fibrillation, the normal cycle of electrical impulses in your heart is interrupted. This leads to a fast, chaotic heart rhythm and poor movement of blood from your atria to your lower chambers .
There are three main types of atrial fibrillation.
- Paroxysmal Afib lasts less than one week and usually stops on its own without treatment.
- Persistent Afib lasts more than one week and needs treatment.
- Long-standing persistent Afib lasts more than a year and is sometimes difficult to treat.
Afib, if untreated, can lead to a stroke and other serious medical complications. Thats why its important to learn the symptoms and talk with your healthcare provider about your personal risk factors.
You May Like: Sore Throat And Sinus Pressure
First Phase: Analysis Of State
We build datasets for the training and evaluation of our six AI models by randomly sampling patients and ECGs in terms of age and sex. In the training set we include 5,337 ECGs from the AF group, with a maximum of five ECGs per patient. All the ECGs are recorded before the first event of AF. For validation and test sets we consider a smaller time window that contains ECGs collected between 2 months and 1 week before the first AF. In the validation set we include 85 ECGs, with a maximum of five ECGs per patient, while in the test set we include all the ECGs available in the specified time window, from a set of 60 patients randomly sampled. SR ECGs in the training and validation sets for the AF group present a median age of 79 years and 77 years , respectively. In the test set, the median age of AF patients is 82.5 years . We specify the median age of patients and not ECGs because, for each patient in the test set, we aggregate the AF scores related to their ECGs and provide a unique score representing their own risk of developing AF.
Table 1 Comparison of AUC results achieved for different models, according to different aggregation rules.Table 2 Comparison of AUC results achieved for different models, according to different scenarios.Table 3 Comparison of the performances obtained for different models, in the scenario of balancing distributions.
Af Pathophysiology And Natural History
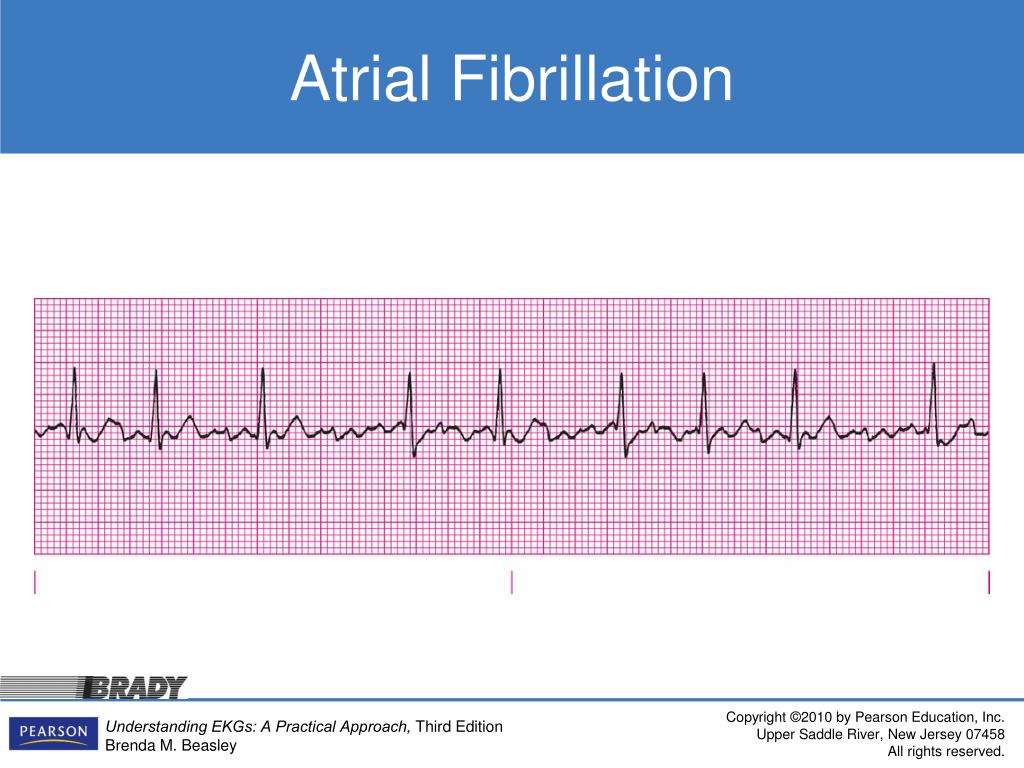
AF is a progressive disease that becomes more difficult to treat with increasing duration. This characteristic is attributed to the occurrence of electrical, contractile, and structural remodelling of the atria, which creates a fertile environment for the propagation of AF. Most frequently, AF occurs in the setting of underlying heart disease, which includes coronary artery disease, hypertension, valve disease, congestive heart failure, and thyroid dysfunction. In 1530% of patients, however, no underlying disease is demonstrable this is termed lone AF.
As AF was first recognized, its underlying aetiology has been a subject of great interest. The three primary proposed mechanisms include one or more rapidly discharging, spontaneously active, atrial ectopic foci a single re-entry circuit and multiple functional re-entrant circuits. The multiple wavelet hypothesis, as formulated by Moe et al. and experimentally confirmed by Allessie et al.,, until recently was generally accepted. Recent observations, however, have challenged this hypothesis. Optical mapping studies of AF in sheep hearts point to a primary local generator as being either an ectopic focus or a small re-entry circuit, implying that both concepts may, indeed, play a role in AF maintenance.
Recommended Reading: Best Medicine For Sinus And Cold