C Laboratory Tests To Monitor Response To And Adjustments In Management
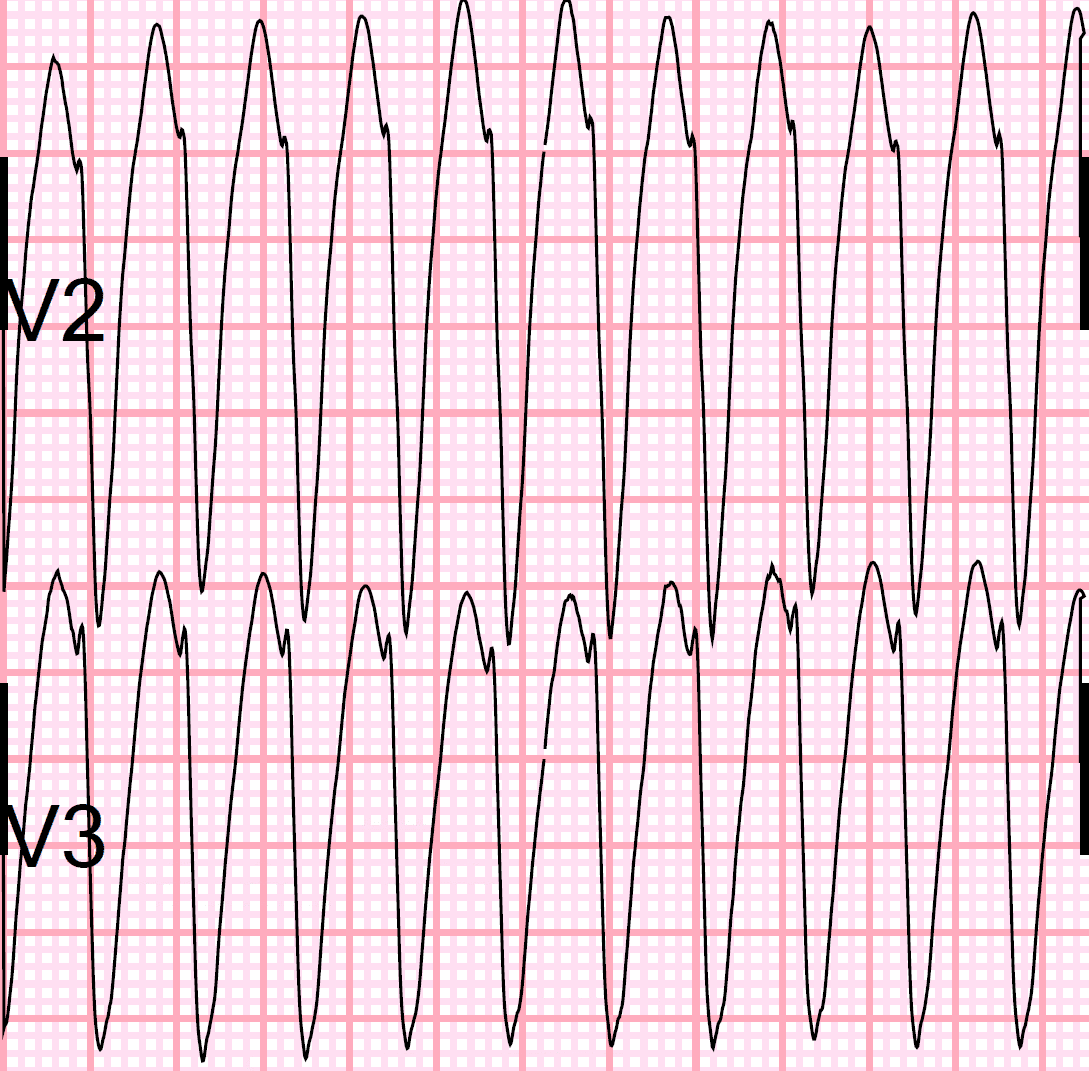
Wide complex tachycardia related to preexcitation
A special consideration is WCT due to anterograde conduction over an accessory pathway. One such example would be antidromic atrioventricular reciprocating tachycardia , where the impulse travels anterogradely over an accessory pathway , and then uses the normal His-Purkinje network and AV node for retrograde conduction back up to the atrium.
Because an accessory pathway inserts directly into ventricular myocardium, the resulting QRS complex during antidromic AVRT is generated by muscle-to-muscle spread propagating away from the ventricular insertion site, rather than via His-Purkinje spread, and therefore meets all the QRS complex morphology criteria for VT. This is one SVT where the QRS complex morphology exactly mimics that of VT.
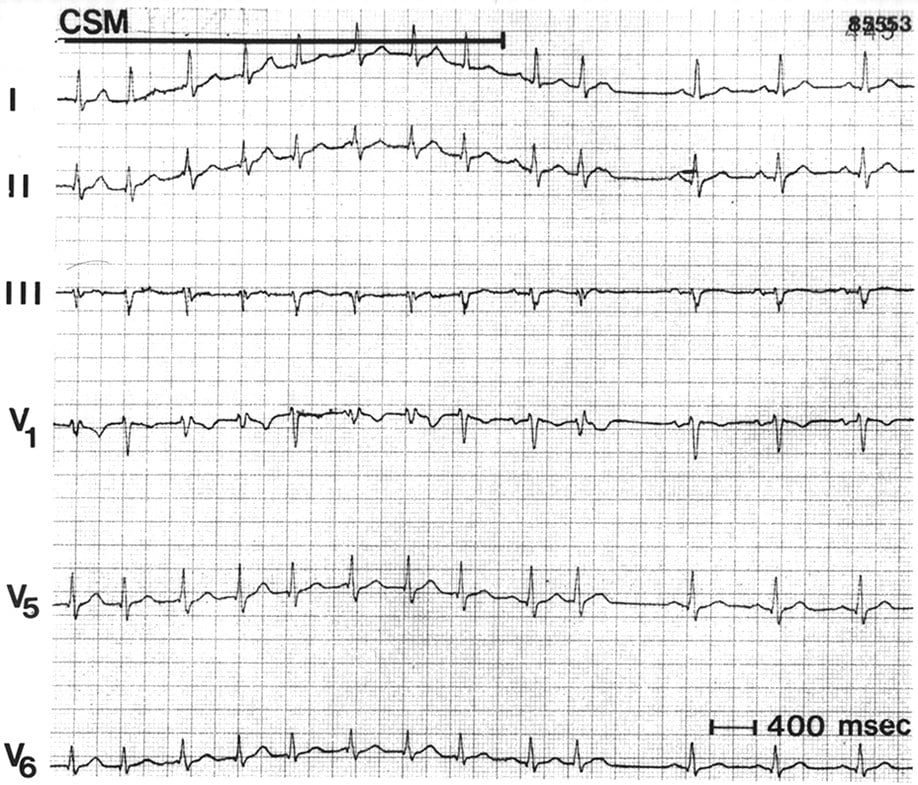
However, such patients are usually young, do not have associated structural heart disease, and most importantly, show manifest preexcitation during sinus rhythm. The pattern of preexcitation in sinus rhythm will be exactly reproduced during antidromic AVRT. Carotid massage and adenosine will terminate this WCT by causing transmission block in the retrograde limb .
Wide complex tachycardia due to bundle branch reentry
Wide complex tachycardia in the setting of metabolic disorders
Wide complex tachycardia related to rapid ventricular pacing
Ii Diagnostic Confirmation: Are You Sure Your Patient Has Wide Qrs Tachycardia
What determines the width of the QRS complex?
The clinical situation that is commonly encountered is when the clinician is faced with an electrocardiogram that shows a wide QRS complex tachycardia , and must decide whether the rhythm is of supraventricular origin with aberrant conduction , or whether it is of ventricular origin . It is important to note that all the analyses that help the clinician distinguish SVT with aberrancy from VT also help to distinguish single wide complex beats .
The width of the QRS complex, both with aberrancy and during VT, can vary from patient to patient. Scar tissue, as seen in patient with prior myocardial infarctions or with cardiomyopathy, may further slow intramyocardial conduction, resulting in wider QRS complexes in both situations.
During VT, the width of the QRS complex is influenced by:
Ventricular Or Supraventricular Tachycardia
Regular wide-complex tachycardia can be either ventricular tachycardia or supraventricular tachycardia. Ventricular tachycardia originates from the left ventricle, the left ventricular outflow tract, the right ventricle or the right ventricular outflow tract. In contrast, wide-complex supraventricular tachycardia arises from aberrant conduction in bundle branch block or, rarely, in an accessory bundle .
Clinical symptoms are not reliable in the differentiation between ventricular tachycardia and supraventricular tachycardia. The patients age might be helpful: the older the patient, the more probable is ventricular tachycardia. Haemodynamics as shown in the two examples above are not reliable markers. In contrast, the patients cardiovascular history might be helpful: for example, if an ischaemic or structural heart disease, previous myocardial infarction, congestive heart failure, a family history of sudden cardiac death is known, ventricular tachycardia is more probable than supraventricular tachycardia. In supraventricular tachycardia with aberration, previous ECGs often show a bundle branch block pattern with morphology identical to that of a wide-complex tachycardia, or evidence of Wolff-Parkinson-White syndrome , and the patients history often includes recurrent paroxysmal tachycardia with sudden onset and termination with vagal manoeuvres or adenosine.
Don’t Miss: What Relieves Sinus Pain And Pressure
A Different Approach The Griffith Algorithm
Recognising the high prevalence of VT and the limited number of typical aberrancies allowed by the conduction system, Griffith et al. proposed criteria, which function in a manner counter to the algorithms above each ECG is analysed for V1 and V6 criteria consistent with aberration.20 If the criteria for aberration are not found, VT is assumed. As the algorithm defaults to VT, its sensitivity can be excellent, but specificity suffer, both in the original paper and in subsequent evaluation.16,17,20 Of note, right ventricular outflow tract tachycardias are frequently misclassified as SVT by this algorithm, and should be evaluated with other criteria by users of this algorithm.
What Is Sinus Arrhythmia
Sinus arrhythmia is a kind of arrhythmia . For the most common type of sinus arrhythmia, the time between heartbeats can be slightly shorter or longer depending on whether youre breathing in or out. Your heart rate increases when you breathe in and slows down when you breathe out. This kind of arrhythmia is considered normal. Its usually a sign that your heart is healthy.
Also Check: How Does A Doctor Diagnose A Sinus Infection
A Wide Qrs Tachycardia With Three Distinct Left Bundle Branch Block Morphologies In A Patient With Sinus Rhythm With Left Bundle Branch Block: What Is The Mechanism
DOI: 10.19102/icrm.2021.121007
ABSTRACT.The differential diagnosis for a wide complex tachycardia includes all causes of supraventricular tachycardia with bundle branch block or all causes of SVT with antegrade pre-excitation by bystander involvement of any accessory pathways, myocardial or bundle brunch ventricular tachycardia, and antidromic and other pre-excited reciprocating tachycardias. We present a case of wide complex QRS tachycardia with a left bundle branch block QRS morphology.
KEYWORDS.Idiopathic ventricular tachycardia, left bundle branch morphology, left bundle branch block tachycardia, left and right cusp commissure, preferential conduction.
The authors report no conflicts of interest for the published content.Manuscript received December 24, 2020. Final version accepted March 31, 2021.Address correspondence to: Ozcan Ozeke, MD, Salk Bilimleri Üniversitesi, Ankara ehir Hastanesi, Kardiyoloji Klinigi, Ankara 06800, Turkey. Email: .
Qrs Prolongation In Patients Without Atrial Fibrillation
Asymptomatic QRS prolongation
The relation between QRSd and morbidity/mortality varies depending on age. Young, asymptomatic patients without cardiovascular disease have normal life expectancy despite QRS prolongation, in the form of a LBBB or right bundle block branch . In contrast, QRS prolongation among older asymptomatic patients portends worse outcomes as demonstrated in the Swedish Primary Prevention Study. Among 7392 middle-aged men, subjects with LBBB were more likely to progress to complete heart block and had greater all-cause mortality over the 28-year follow-up. Similarly, subjects with RBBB were more likely to progress to a high-degree AV block or need a pacemaker implantation compared with those without a BBB . Similar results were found with a 2.5- to 10-fold increase in risk for sudden cardiac death among patients with prolonged QRS in two large observational studies.,
Cardiovascular disease and QRS prolongation
You May Like: Nasal Spray For Sinus Cold
B Physical Examination Tips To Guide Management
The hallmark of VT is ventriculoatrial dissociation , the following examination findings , when clearly present, clinch the diagnosis of VT. Absence of these findings is not helpful, since VT can show VA association . Of course, such careful evaluation of the patient is only possible when the patient is hemodynamically stable during VT any hemodynamic instability should prompt urgent or emergent cardioversion. Therefore, measurement of vital signs and a thorough but rapid physical examination are vital in deciding on the initial approach to the patient with WCT. If the patient is conscious and cardioversion is decided upon, it is strongly recommended that sedation or anesthesia be given whenever possible prior to shock delivery.
Table II.
Findings on Physical Examination to help distinguish causes of WCT
Recognition of intermittent cannon A waves on the jugular venous waveform during ongoing WCT is an important physical examination finding because it implies VA dissociation, and can clinch the diagnosis of VT. The recognition of variable intensity of the first heart sound can similarly be another clue to VA dissociation, and can help make the diagnosis of VT.
General approach to the ECG showing a WCT
Table III shows general ECG findings that help distinguish SVT with aberrancy from VT.
Table III.
General ECG findings that help distinguish SVT with aberrancy from VT
Qrs Prolongation In Patients With Atrial Fibrillation
Even though AF and complete BBB are individually recognized as important predictors of morbidity and mortality,,, the relationship between QRSd and morbidity/mortality in patients with AF is poorly studied, especially among those with mild degrees of QRS prolongation or those without HF. Among the 669 patients from the In-CHF database, the presence of a complete LBBB and AF was associated with increased 1-year mortality and 1-year hospitalization . The large cohort and long-term follow-up of the AFFIRM trial overcome previous limitations of smaller studies with shorter follow-up, while demonstrating similar increases in morbidity and mortality with QRS prolongation among patients with AF. Such findings, already extensively demonstrated in sinus rhythm, may have clinical implications. It reinforces for instance the theoretical ground for the benefit of biventricular pacing in AF patients, for whom the benefits of cardiac resynchronization have been much less studied than for those in sinus rhythm.
Furthermore, two novel findings with potential clinical implications arise from our analysis.
Secondly, our analysis suggests that a prolonged QRSd 120 ms in non-HF patients with AF is associated with worse outcomes compared with those with normal QRSd. These results correlate with findings from previous studies among patients without AF as described above. Our analysis further extends such findings to the type of patients with AF enroled in AFFIRM.
Read Also: Can You Drink On Sinus Infection Antibiotics
Doses And Handling Of Adenosine
Adenosine is injected rapidly in a peripheral venous catheter or central venous catheter followed by flushing with 20 ml saline. The injection may be repeated with doubled dose . Heart transplanted individuals are particularly sensitive and should therefore receive only half the dose in a peripheral venous catheter.
Adenosine is only given during continuous ECG monitoring and a defibrillator must be close at hand. Adenosine is contraindicated in high-degree AV block , sick sinus syndrome , pronounced hypotension, unstable angina pectoris and decompensated heart failure.
Most patients experience chest discomfort during adenosine administration. Anxiety and flushing are also common. Obstructive pulmonary disease is a relative contraindication to adenosine. Theophylline and caffeine reduce sensitivity to adenosine. Heart transplanted patients, and those on dipyramidole, have increased sensitivity. Adenosine doses in pediatric population is weight-based.
Recall that in case of hemodynamic instability, electrical cardioversion is always the first choice.
Analysis Of Atrial Activity
Analyzing atrial activity during tachyarrhythmias is crucial but difficult. P-waves may be invisible or visible and in the latter case, they may have an abnormal appearance. If the ventricles and the atria are activated simultaneously, the P-wave will be hidden in the QRS complex. If atria and ventricles are not activated simultaneously, but separately, the P-wave may be visible. The direction of the P-wave depends on the origin of the impulse. If the impulse is discharged near the atrioventricular node, atrial activation will proceed in the opposite direction and the P-wave will be retrograde in leads normally showing a positive P-wave. If the atrial impulse originates near the sinoatrial node, the P-wave will appear normal .
If no P-waves are visible, the primary suspect is AVNRT. If P-waves are visible, the following must be judged:
- Are P-waves positive or retrograde?
- How fast is the atrial rate?
- Where do P-waves occur, in relation to the QRS complexes?
- Are P-P intervals regular? Completely irregular? Irregular but with a repeating pattern?
- Is the number of P-waves equal to the number of QRS complexes?
At very high atrial rates one should suspect atrial flutter or atrial tachycardia. Besides this, the atrial rate is of little help.
Recommended Reading: Northwest Indiana Ent And Sinus Center
What’s The Evidence For Specific Management And Treatment Recommendations
Kindwall, KE, Brown, J, Josephson, ME.. Electrocardiographic criteria for ventricular tachycardia in wide complex left-bundle branch block morphology tachycardias. Am J Cardiol. vol. 15. 1988. pp. 1279-83.
Vereckei, A, Duray, G, Szenasi, G. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. European Heart J. vol. 28. 2007. pp. 589-600.
Brugada, P, Brugada, J, Mont, L. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. vol. 83. 1991. pp. 1649-59.
Vereckei, A, Duray, G, Szenasi, G. New algorithm using only lead aVR for differential diagnosis of wide QRS complex tachycardia. Heart Rhythm. vol. 5. 2008. pp. 89-98.
Goldberger, ZD, Rho, RW, Page, RL.. Approach to the diagnosis and initial management of the stable adult patient with a wide complex tachycardia. Am J of Cardiol. vol. 101. 2008. pp. 1456-66.
Jastrzebski, M, Kukla, P, Czarnecka, D, Kawecka-Jaszcz, K.. Comparison of five electrocardiographic methods for differentiation of wide QRS-complex tachycardias. Europace.. vol. 14. 2012 Aug. pp. 1165-71.
Jastrzebski, M, Sasaki, K, Kukla, P, Fijorek, K. The ventricular tachycardia score: a novel approach to electrocardiographic diagnosis of ventricular tachycardia. Europace.. vol. 18. 2016 Apr. pp. 578-84.
Huemer, M, Meloh, H, Attanasio, P, Wutzler, A. The Lewis Lead for Detection of Ventriculoatrial Conduction Type. Clin Cardiol. vol. 39. 2016. pp. 126-131.
Tachycardia: The Value Of Anamnesis
Anamnesis is as always important. Many tachycardias have a triggering factor, such as physical or emotional stress, coffee consumption, etc. It is always useful to assess whether the tachycardia started abruptly or gradually. This may differentiate several tachycardias. Sinus tachycardia, for example, always starts gradually, whereas AVNRT always starts very abruptly. The patient can determine the start of the arrhythmia in most cases.
Previous medications, comorbidities and precious ECG tracings should all be assessed. The value of this lies in the fact that if there is any precipitating factor, the arrhythmia is likely to be related to that factor. For example, patients on sotalol medication are likely to have ventricular tachycardia patients with previous myocardial infarction are very likely to have ventricular tachycardia if they present with a wide complex tachycardia patients with previous atrial fibrillation are likely to have another episode if they present with an irregular tachycardia and so on.
Don’t Miss: Advil Cold And Sinus Symptoms
Initial Management Of Wide Complex Tachycardias
Hemodynamic status must be assessed immediately because it may be unstable. If there are signs of compromised hemodynamics the patient should be treated with synchronized electrical cardioversion, even before a diagnosis has been established. A wide complex tachycardia is considered as a ventricular tachycardia until proven otherwise, and in the case of affected circulation it is highly likely that the arrhythmia is ventricular tachycardia. Note that some patients with ventricular tachycardia may be hemodynamically stable initially sustained ventricular tachycardias, however, always cause circulatory symptoms. The greater the cardiac function, the less pronounced the symptoms.
Unconscious and pulselss patients are managed with advanced cardiac life support.
If the patient is hemodynamically stable, one may study the ECG carefully and attempt treating the arrhythmia pharmacologically. Pharmacological treatment alternatives have been discussed previously. A flow-chart with treatment and management is presented in Figure 5.
Specific Noteworthy Ventricular Tachycardias
Three types of VT are particularly amenable to treatment by drugs, catheter ablation or both. These largely benign forms of VT are particularly important their presence, in the setting of a structurally normal heart, is a contraindication for ICD implantation.21 Diagnosis of these forms of VT is more difficult than the VT-related to structural heart disease, because the QRS duration is comparatively shorter, VA conduction is often present , and many other criteria fail to distinguish these VTs from SVT . An additional VT-type, bundle branch re-entry , usually has an appearance indistinguishable from LBBB SVT and thus belongs in the general category of VTs that are difficult to distinguish from SVT. While BBR VT is also quite amenable to catheter ablation, it generally occurs in patients with significant structural heart disease thus most patients with BBR VT also warrant ICD therapy.
Criteria Incorrectly Suggests Ventricular Tachycardia in this Patient with Right Bundle Branch Block Supraventricular Tachycardia and Prior Myocardial Infarction
A: QRS duration 140 ms B: QRS configuration is qR C: R/S ratio in V6 < 1 D: absent RS in precordial leads E: aVR with monophasic R wave F: QRS onset to peak in lead II < 50 ms .
You May Like: Will Z Pack Treat A Sinus Infection
Vagal Stimulation For Diagnosis And Treatment Of Tachycardia
One may always try vagal stimulation before administration of adenosine. Commonly used methods are carotid massage, Valsalva maneuver, and splashing cold water on the face . Carotid massage is performed with the patient in the supine position and head rotated slightly away from the side being massaged. The carotid artery is massaged, at the level of the larynx, with two fingers. The massage is best performed with a circulating movement for 10 to 20 seconds. It may be repeated on the opposite side. Correctly performed, this induces a baroreceptor reflex which increases vagal stimulation to the heart and thus increases the block in the AV node. This may terminate 5 to 20% of AVNRT and AVRT.
Vagal stimulation may be used as a diagnostic tool as well. Because of the increased AV nodal block, the ventricular rate is lowered and this may clarify the irregularity of atrial fibrillation it may demask the characteristics sawtooth-formed baseline in atrial flutter as well. Note that some individuals have very sensitive baroreceptors in the carotid artery and these individuals may be affected by bradycardia or hypotension upon stimulation.
Enhancing Healthcare Team Outcomes
Although the management of WCT is complex, given its broad differential and numerous etiologies, this article emphasizes a multidisciplinary team approach for ventricular arrhythmias because they are the most common cause of WCT. A multidisciplinary team will be required during both the in-patient and outpatient setting.
This team usually consists of emergency room physicians, cardiologists, cardiac electrophysiologists, ICU intensivists, clinical pharmacists, nurses, nutrition specialists, case managers, cardiac rehabilitation specialists, psychologists, and primary care physicians. It is beneficial to have multiple team members involved as it can optimize a patients care and improve their quality of life. Typically while the patient is in the hospital, their care is predominantly coordinated by the primary cardiologist in conjunction with a cardiac electrophysiologist who will decide on optimal treatment options taking into consideration the patients risk factors and comorbidities. Once these patients are discharged home from either the hospital or rehabilitation centers, they will still require a multidisciplinary approach to facilitate their care.
Read Also: Good Things For Sinus Infections
What Causes Sinus Arrhythmia
Providers separate different kinds of sinus arrhythmia based on their causes.
Respiratory sinus arrhythmia
Its normal to have respiratory sinus arrhythmia simply because youre breathing. When you take a breath, your heart rate goes up. When you breathe out, it slows down.
The time between each heartbeat is known as the P-P interval. In most people, theres a slight variation of less than 0.16 seconds. In cases of respiratory sinus arrhythmia, the P-P interval will often be longer than 0.16 seconds when the person breathes out.
Nonrespiratory sinus arrhythmia
In EKG results, nonrespiratory sinus arrhythmia can look like respiratory sinus arrhythmia. But people with this type usually:
- Had a head or neck injury.
- Took too much digoxin .
- Have heart disease.
Ventriculophasic sinus arrhythmia
Providers can identify ventriculophasic sinus arrhythmia by looking at the electrocardiogram results. People with this kind of sinus arrhythmia usually have third-degree AV block.