Why It Is Important To Do This Review
Many trials have studied longterm treatment with diverse antiarrhythmic drugs for maintaining sinus rhythm, sometimes compared to placebo and sometimes compared to other antiarrhythmic drugs. Attempts to summarise this evidence in systematic reviews of trials or metaanalyses have been incomplete. They were combined in a narrative review trials using different antiarrhythmics and with very dissimilar lengths of treatment were pooled together and outcomes other than sinus rhythm maintenance were not evaluated . Consequently, we planned to conduct a more exhaustive systematic review of randomised controlled trials studying the longterm use of antiarrhythmic drugs to maintain sinus rhythm and aimed to determine their effects not only on the recurrence of atrial fibrillation but also on other important clinical outcomes. After the first publication of this review, another metaanalysis on the same subject was published by Freementle et al . This metaanalysis employed nonclassical statistical methods and it is not known if these methods are better or worse than the classical metaanalytical approach.
After the first publication of this review in 2007, several new randomised controlled trials have been published. They have been systematically searched, assessed and, when found adequate, included in the successive updates of this review.
What Happens During The Procedure
While you are asleep, the doctor will use the cardioverter machine to quickly deliver specific amounts of energy to your heart through the cardioversion patches. The shock interrupts the abnormal electrical rhythm and restores a normal heart rhythm. It may take several shocks to get the rhythm back to normal.
How Do I Prepare For An Electrical Cardioversion
Talk with your healthcare provider about what you should do to get ready for your electrical cardioversion. You may need to avoid eating or drinking anything before midnight of the day of your procedure.
Follow your healthcare provider’s instructions about what medicines to take before the procedure. This includes any medicines to prevent abnormal rhythms. Don’t stop taking any medicine unless your healthcare provider tells you to do so. You might need blood tests before the procedure to make sure the procedure is safe to do.
If you are at higher risk of blood clots, your healthcare provider may want you to take anti-clotting medicine. These are commonly taken for several weeks before and after the procedure. Not everyone needs this medicine, but some people do. You are likely to need anti-clotting medicine if your abnormal rhythm has lasted more than 48 hours or if you have had a blood clot in the past.
Your healthcare provider may want a transesophageal echocardiography test before the procedure. This test is a special kind of ultrasound. A thin, flexible tube is put down your throat and into your esophagus. Here, the tube is close to your heart. It lets your healthcare provider see if you have any blood clots in the heart. Your cardioversion will be delayed if a clot is found. You’ll likely need to take blood thinner medicine for a while until your risk of clots is low. It’s important to take this medicine exactly as your healthcare provider tells you.
Don’t Miss: Why Do I Get Sinus Headaches Everyday
Ablate And Pace Strategy
There are a few small randomised clinical trials comparing pharmacological rate control and permanent pacing with complete AV node catheter ablation in patients with HF. These trials showed a benefit of an ablate and pace strategy in terms of symptom relief, HF hospitalisations and mortality . AV node ablation solves the problem of rapid ventricular response in AF, which aggravates symptoms and HF.
Catheter ablation of the AV node and permanent pacing should be considered if pharmacological rate control fails . The optimal choice of pacemaker type or pacing mode is still unclear.
Right ventricular or biventricular pacing is the next question which should be answered in the future. There are limited data suggesting an advantage of biventricular pacing versus right ventricular pacing in HF patients.
How Is Atrial Fibrillation Treated
The goals of treatment for atrial fibrillation include regaining a normal heart rhythm , controlling the heart rate, preventing blood clots and reducing the risk of stroke.
Many options are available to treat atrial fibrillation, including lifestyle changes, medications, catheter-based procedures and surgery. The type of treatment that is recommended for you is based on your heart rhythm and symptoms.
Recommended Reading: Sudafed Sinus Congestion 30 Mg
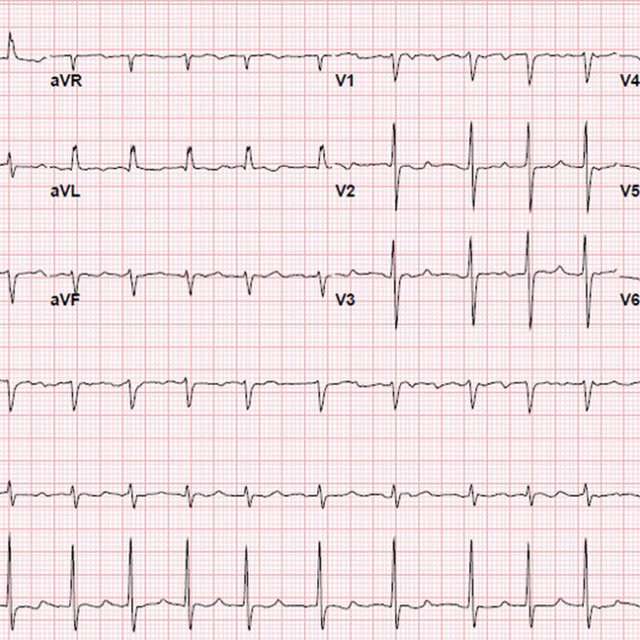
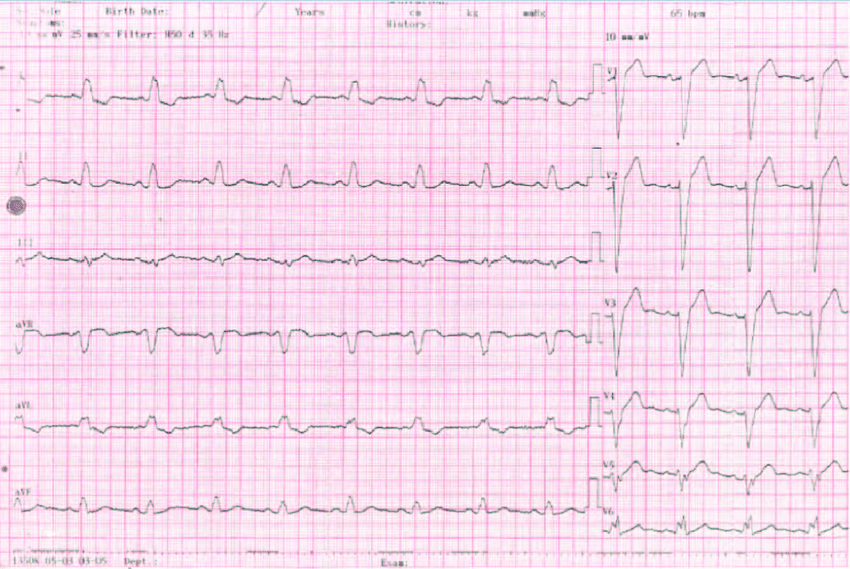
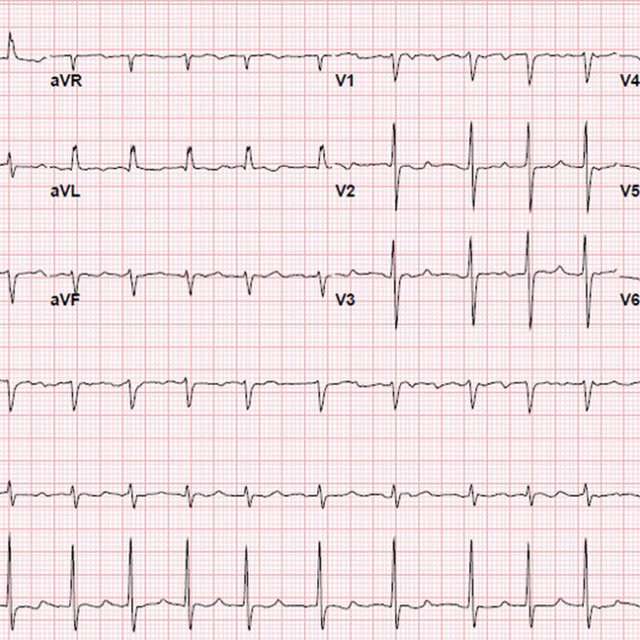
Prediction Of Successful Cardioversion And Af Recurrence By Dacl
Patients successfully restored to sinus rhythm had a mean DACL in lead V1 of 153 ± 15 ms v 158 ± 21 ms in the patients who had a primary failure of cardioversion . Comparable data for the oesophageal lead was 148 ± 15 ms vs. 151 ± 13 ms .
Among patients who had been cardioverted, DACL was non-significantly longer in those who remained in sinus rhythm at 6 weeks than those who had relapsed to AF by this point . Utilising the shortest DACL value from either lead did not improve discriminatory power . DACL did not correlate with left atrial diameter, with a Spearman R = 0.25 for DACL from lead V1 and R = -0.04 from the oesophageal lead .
Center For Atrial Fibrillation
Cleveland Clinic’s Center for Atrial Fibrillation offers comprehensive treatment for patients with atrial fibrillation.Specialists from cardiology, cardiac surgery, cardiac imaging, arrhythmia research, emergency medicine, neurology and geriatric medicine combine their expertise to tailor individual approaches for their patients.
When you come to Cleveland Clinics Center for Atrial Fibrillation, you will receive care from some of the leading specialists in the world. Many of our physicians participate in the research and development of the newest treatments.
Our physicians participate in scientific and clinical investigations focused on improving our understanding of the underlying causes of atrial fibrillation, in order to increase the long-term efficacy of available treatment options.
Doctors vary in quality due to differences in training and experience hospitals differ in the number of services available. The more complex your medical problem, the greater these differences in quality become and the more they matter.
Clearly, the doctor and hospital that you choose for complex, specialized medical care will have a direct impact on how well you do. To help you make this choice, please review our Miller Family Heart, Vascular & Thoracic Institute Outcomes.
You May Like: Relieve Sinus Pressure In Ears
How Long Does The Cardioversion Procedure Last
The procedure itself lasts only a few minutes. However, the preparation and recovery time for the procedure may add a few hours to your appointment. Please plan to stay at Cleveland Clinic 4 to 6 hours for your appointment.
If you have an appointment with your physician on the same day of the procedure, please plan to spend the entire day at Cleveland Clinic.
Success Rate Of Cardioversion
Electrical Cardioversion is considered a standard, routine, low risk treatment option, particularly for recent onset A-Fib patients. If your A-Fib has just started, it may be a momentary aberration and an Electrical Cardioversion may correct it.
Cardioversion has a very high initial success rate, returning up to 95% of A-Fib patients to NSR.
While the conversion rate is high, recurrence of A-Fib is high too. Cardioversion doesnt prevent future episodes of A-Fib. As few as 23% of patients remain in normal sinus rhythm for more than one year post-procedure. For most, their A-Fib returns within the first five days.4
You May Like: Where To Get Antibiotics For Sinus Infection
Rate Control Therapy In Atrial Fibrillation
Rate control is the first-line therapy in elderly patients. Usually, this is sufficient to control the symptoms in symptomatic patients and it is also the treatment choice in asymptomatic patients. Rate control allows AF to persist, controlling the heart rate with medications that slow down the conduction through the atrioventricular node.
The evidence concerning which is the best type of rate control and its intensity level is unclear.
Acute rate control
Acute rate control refers to an acute slowing of the heart rate where haemodynamic stability is achieved. The underlying causes of a high heart rate in new-onset AF could be acute infection, anaemia, endocrine imbalance, pulmonary thromboembolism, etc. If high sympathetic tone is suspected as a reason for the high heart rate, then beta-blockers or non-dihydropyridine calcium channel blockers are preferred over digoxin.
If the patient has a left ventricular ejection fraction < 40%, then beta-blockers and/or digitalis are preferred over CCB, because CCB have negative inotropic effects .
In critically ill patients and those with severely impaired LV systolic function, intravenous amiodarone can be used where excess heart rate is leading to haemodynamic instability . Urgent cardioversion should be considered in haemodynamically compromised patients .
Long-term rate control
Strict versus lenient rate control
What Should I Wear
- Wear comfortable, easy-to-fold clothes when you come to the hospital. You will wear a hospital gown for the procedure.
- Do not wear makeup or nail polish.
- Do not use deodorant, powder, cream or lotion on your back or chest. These products can cause problems with the adhesive pads that are used during the procedure.
- Please leave all jewelry , watches and valuables at home.
You May Like: Sinus Allergies At The Beach
Prediction Of Successful Restoration Of Sinus Rhythm
Sinus rhythm was restored in 32 of 37 patients. Patients who failed cardioversion tended to have larger left atria and, paradoxically, a longer atrial fibrillatory cycle length. Neither parameter however, nor the combination of the two, proved an important predictor of outcome. Successful cardioversion is dependent upon cardioversion technique and transthoracic impedance, which is influenced by body size, obesity and the presence of pulmonary disease. Some data suggest left atrial enlargement decreases the probability of cardioversion while others do not. Thus although there may be a contribution of electrical and structural remodeling to cardioversion rates, the major determinants are likely to be procedural.
What Is A Cardioversion
Cardioversion is a corrective procedure where an electrical shock is delivered to the heart to convert, or change, an abnormal heart rhythm back to normal sinus rhythm. Most elective or “non-emergency” cardioversions are performed to treat atrial fibrillation or atrial flutter , non-life threatening abnormal rhythms in the top of the heart. Cardioversion is also used in emergency situations to correct an abnormal rhythm when it is accompanied by faintness, Low Blood Pressure, chest pain, difficulty breathing, or loss of consciousness.
The purpose of the cardioversion is to interrupt the abnormal electrical circuit in the heart and to restore a normal heartbeat. The delivered electrical shock causes all the heart cells to contract simultaneously, thereby interrupting and terminating the abnormal electrical rhythm without damaging the heart. The heart’s electrical system then restores a normal heartbeat.
Also Check: Puffy Under One Eye Sinus
What Happens After An Electrical Cardioversion
Ask your healthcare provider about what to expect. You will likely:
- Wake up 5 to 10 minutes after the procedure
- Be closely watched for signs of complications for several hours
- Feel sleepy for several hours after the cardioversion. Arrange to have someone drive you home
- Go home the same day as the procedure
- Have some redness or soreness on your chest that lasts for a few days
Ask your healthcare provider about what medicines you’ll need to take when you get home. Many people need to take an anti-clotting medicine like warfarin or another blood thinner. Some people also need medicines to prevent abnormal heart rhythms. Take all your medicines exactly as your healthcare provider tells you. Tell your healthcare provider right away if any of your symptoms come back.
What Are The Risks Of Cardioversion
If you have atrial fibrillation, blood clots can form in your hearts left atrium. Cardioversion may knock loose a blood clot in your left atrium. If the clot travels to your brain, it can cause a stroke. To avoid this, your doctor may give you medicine to make your blood less likely to form blood clots. If your doctor gives you the medicine, youll need to take it for 2 to 3 weeks before the procedure. Transesophageal echocardiography is often used to check for the presence of blood clots before this procedure.
- If you have an electrical cardioversion, the skin on your chest or back where the paddles are applied may become irritated. Your doctor can tell you about creams to make your skin feel better.
- Cardioversions dont always bring back normal heart rhythms. If normal rhythms dont return, you may need medicines, a pacemaker or an implantable cardioverter defibrillator .
Also Check: Prescription Antibiotics For Sinus Infection
Restore A Normal Heart Rhythm And Prevent Relapses
Sometimes, when you have an episode of atrial fibrillation, the normal rhythm is restored without treatment. If this doesnt happen, or if you have symptoms during your atrial fibrillation episodes, your doctor may suggest you restore your heart rhythm back to a normal rhythm . This is what we call rhythm control.
When choosing the rhythm control strategy, there are two options in restoring the normal sinus rhythm: with medication and with electrical cardioversion.
Before you have a cardioversion, whether this is an electrical or a pharmacological one, your physician may require you to take anticoagulants , for at least 3 weeks before the procedure. Otherwise, your doctor may want to rule out any blood clots within the heart by performing a specific imaging exam called transoesophageal echo before the cardioversion. You will also need to continue your anticoagulant drugs for at least 4 weeks after the cardioversion to reduce your risk of stroke. Depending on your overall risk of stroke your doctor may ask you to continue taking a blood-thinner for the rest of your life.
What Is The Best Strategy To Follow In Very Old Patients With Atrial Fibrillation: Rate Or Rhythm Control
Assoc. Prof Lidija Poposka
Management of atrial fibrillation in the rapidly growing population of older patients involves a comprehensive strategy that includes consideration of their comorbidities, functional and social status. Activity level and medication tolerance are different in this category of patients and expectations are focused on quality of life and symptom relief. Invasive methods, such as catheter ablation, are the new frontier of treatment for maintaining sinus rhythm in this population with complication rate comparable to younger patients.
You May Like: Is Zinc Good For Sinus Infections
Rate Or Rhythm Control In Heart Failure Patients
HF and AF are conditions in older patients that often coexist and promote each other. The danger of proarrhythmia and the negative inotropic effect of many antiarrhythmic drugs are limiting factors for their use in HF patients. However, maintenance of sinus rhythm is possibly most important in this subgroup of patients, due to the positive effect of sinus rhythm on functional status and the possible reduction in mortality . As such, ablation has been proposed as a more efficacious way of achieving sinus rhythm. Most of the positive results of ablation in HF patients stem from the CASTLE-AF study . Ablation resulted in a lower AF burden and improved ejection fraction in the ablation group. However, these data cannot simply be transferred to elderly patients, given that the average age of patients in the CASTLE-AF study was 64 years. Subgroup analyses suggested that patients with advanced HF did not benefit from an ablation procedure. This study contributed to the definition of successful ablation as lowering AF burden instead of prevention of AF recurrence .
What Are The Dangers Of Atrial Fibrillation
Some people live for years with atrial fibrillation without problems. However, atrial fibrillation can lead to future problems:
- Because the atria are beating rapidly and irregularly, blood does not flow through them as quickly. This makes the blood more likely to clot. If a clot is pumped out of the heart, it can travel to the brain, resulting in a stroke, or to the lungs, causing a pulmonary embolism. People with atrial fibrillation are 5 to 7 times more likely to have a stroke than the general population. Clots can also travel to other parts of the body , and cause other damage.
- Atrial fibrillation can decrease the hearts pumping ability. The irregularity can make the heart work less efficiently. In addition, atrial fibrillation that occurs over a long period of time can significantly weaken the heart and lead to heart failure.
- Atrial fibrillation is associated with an increased risk of stroke, heart failure and even death.
Read Also: Sinus Infection Vs Flu Vs Cold
Lower Your Pulse Or Reset Your Heart Rhythm
Most people who have only have treatment to slow down their heartbeat. The aim of this treatment to control the heart rate is to reduce the hearts workload and relieve bothersome symptoms. Beta blockers are typically used to lower the resting heart rate to less than 110 beats per minute at first. If that isnt enough to relieve the symptoms, doctors can try to lower the resting heart rate further, either by using a higher dose of the same medication or using additional medications.
Another option is to try to restore the normal sinus rhythm, either with medication or by delivering a small electric shock. The medical term for this is pharmacological or electrical cardioversion. After cardioversion, people typically take medication to stabilize their heart rate and ultimately prevent from recurring.
What Is Electrical Cardioversion
Cardioversion is a procedure used to return an abnormal heartbeat to a normal rhythm. This procedure is used when the heart is beating very fast or irregular. This is called an arrhythmia. Arrhythmias can cause problems such as fainting, stroke, heart attack, and even sudden cardiac death. With electrical cardioversion, a high-energy shock is sent to the heart to reset a normal rhythm. It is different from chemical cardioversion, in which medicines are used to try to restore a normal rhythm.
Normally, a special group of cells begin the electrical signal to start your heartbeat. These cells are in the sinoatrial node. This node is in the right atrium, the upper right chamber of the heart. The signal quickly travels down the heart’s conducting system on the way to the ventricles, the two lower chambers of the heart. As it travels, the signal triggers nearby parts of the heart to contract. This organized pattern helps the heart contract in a coordinated way.
Various problems can disrupt this signaling pathway and lead to abnormal heart rhythms. The heart might beat very quickly, not leaving it enough time to fill with blood between beats. This can prevent your heart from pumping enough blood to the body. Some abnormal heart rhythms raise your risk of stroke. Some also raise the risk of life-threatening rhythms that can lead to sudden death. Cardioversion upsets the abnormal signaling and lets the heart to reset itself back into a normal rhythm.
Recommended Reading: I Think I Have Sinus Infection